 |
Research
UC Irvine's Department of Neurological Surgery has active research activities and research protocols in normal pressure hydrocephalus, neuro-oncology and spinal cord injury.
Some current studies include:
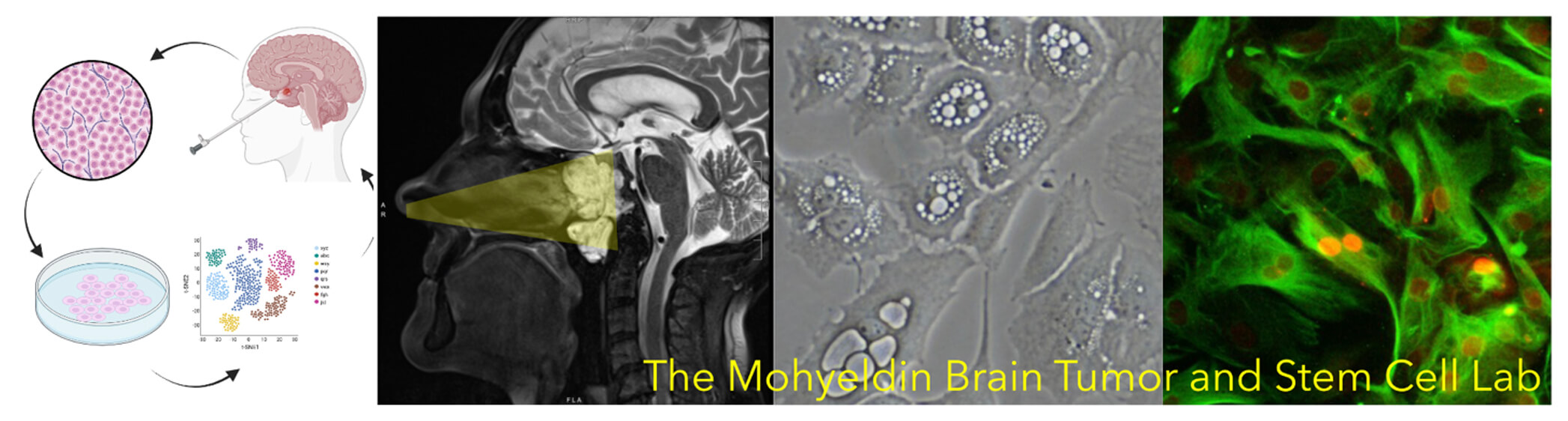
The Mohyeldin Brain Tumor Research Lab
Our research group led by neurosurgeon-scientist Dr. Ahmed Mohyeldin, has a unique philosophy that leverages the utility of thinking about our patients’ medical problems from both a basic science and clinical perspective. We are driven by a fundamental purpose to better elucidate our understanding of brain tumors while also improving the surgical outcomes of the patients that we serve. This unique mindset allows for a synergistic approach to characterize and decipher how brain tumors arise and how they behave, which in turn allows us to discover better therapeutics for our patients. The challenges that we see in the operating room help frame and focus the questions that we are asking in the laboratory and this formula has been critical to our success. Our research focuses on primary tumors of the brain, pituitary gland and skull base. Our groups’ collective expertise in the surgical management of complex brain tumors, cell culture engineering, animal tumor models, cell signaling, computational biology, bioinformatics and spatial-omics allows us to directly utilize brain tumor tissue from the operating room with the consent of our patients for rigorous laboratory investigation. This powerful workflow allows us to study brain tumors up close and probe their complexity directly instead of relying on artificial models or surrogates.
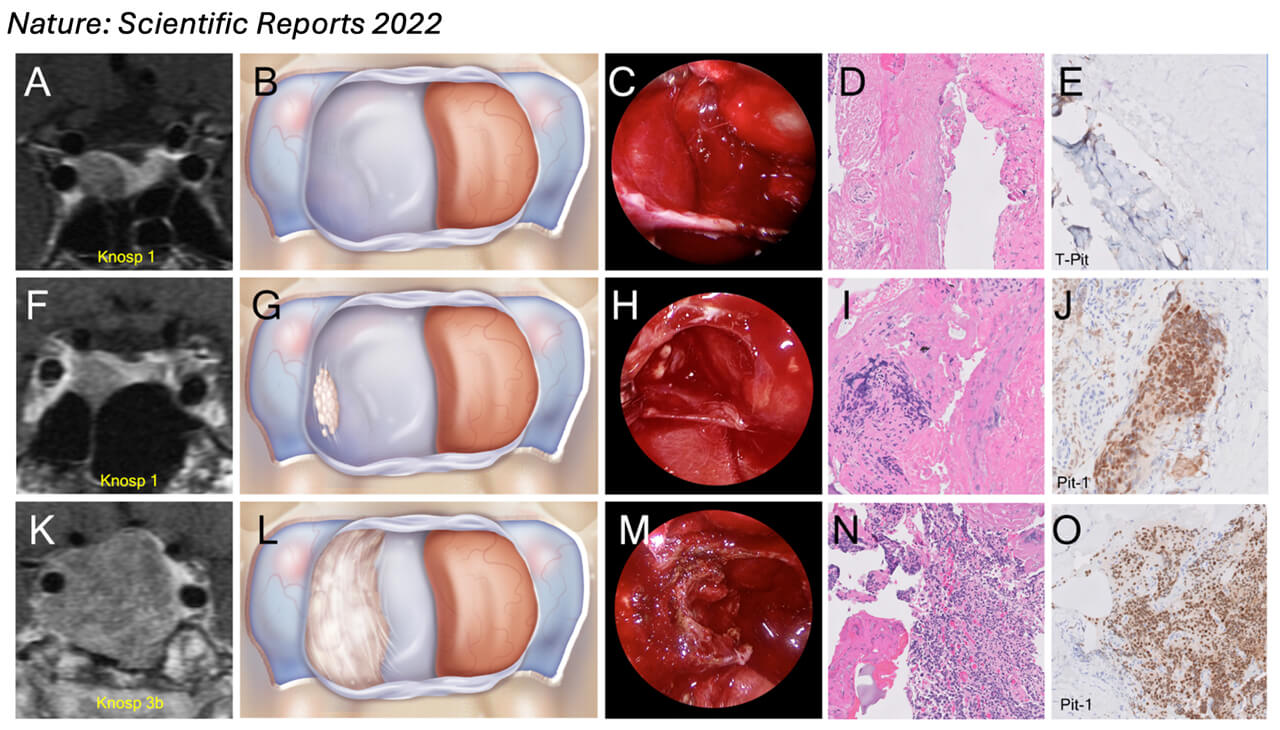
Pituitary Adenoma Research
Our research group remains committed to offering our patients state of the art, advanced, multi-disciplinary endoscopic endonasal surgery for pituitary tumor patients and advancing our understanding pituitary tumors. In a large prospective clinical trial we discovered a pattern of invasion unique to certain pituitary adenoma subtypes that hasn’t been characterized before (Mohyeldin et al. 2022 Nature: Scientific Reports). We also discovered that resection of the medial wall of the cavernous offered durable biochemical remission at unprecedented rates that that previously reported in the literature. In this study we evaluated 107 consecutive primary pituitary adenomas operated on by a single neurosurgeon including 28 corticotroph, 27 gonadotroph, 24 somatotroph, 17 lactotroph, 5 null-cell and 6 plurihormonal. In each case, we performed direct endoscopic intraoperative inspection of the medial wall of the cavernous sinus, which was surgically removed when invasion was visualized. This was performed irrespective of tumor functional status. Medial wall resection was performed in 47% of pituitary adenomas, and 39/50 walls confirmed pathologic evidence of invasion, rendering a positive predictive value of intraoperative evaluation of medial wall invasion of 78%. We show for the first-time dramatic disparities in the frequency of medial wall invasion among pathological subtypes. Somatotroph tumors invaded the medial wall much more often than other adenoma subtypes, 81% intraoperatively and 69% histologically, followed by plurihormonal tumors (40%) and gonadotroph cell tumors (33%), both with intraoperative positive predictive value of 100%.
Removal of the cavernous sinus medial wall was not associated with permanent cranial nerve morbidity nor carotid artery injury, although 4 patients (all Knosp 3-4) experienced transient diplopia. Medial wall resection in acromegaly resulted in the highest potential for biochemical remission ever reported, with an average postoperative day 1 GH levels of 0.96 ug/L and surgical remission rates of 92% based on normalization of IGF-1 levels after surgery (mean = 15.56 months; range 3-30 months). Our findings suggest that tumor invasion of the medial wall of the cavernous sinus may explain the relatively low biochemical remission rates currently seen for acromegaly and illustrate the relevance of advanced intradural surgical approaches for successful and durable outcomes in endonasal pituitary surgery for functional adenomas.
Chordoma Research
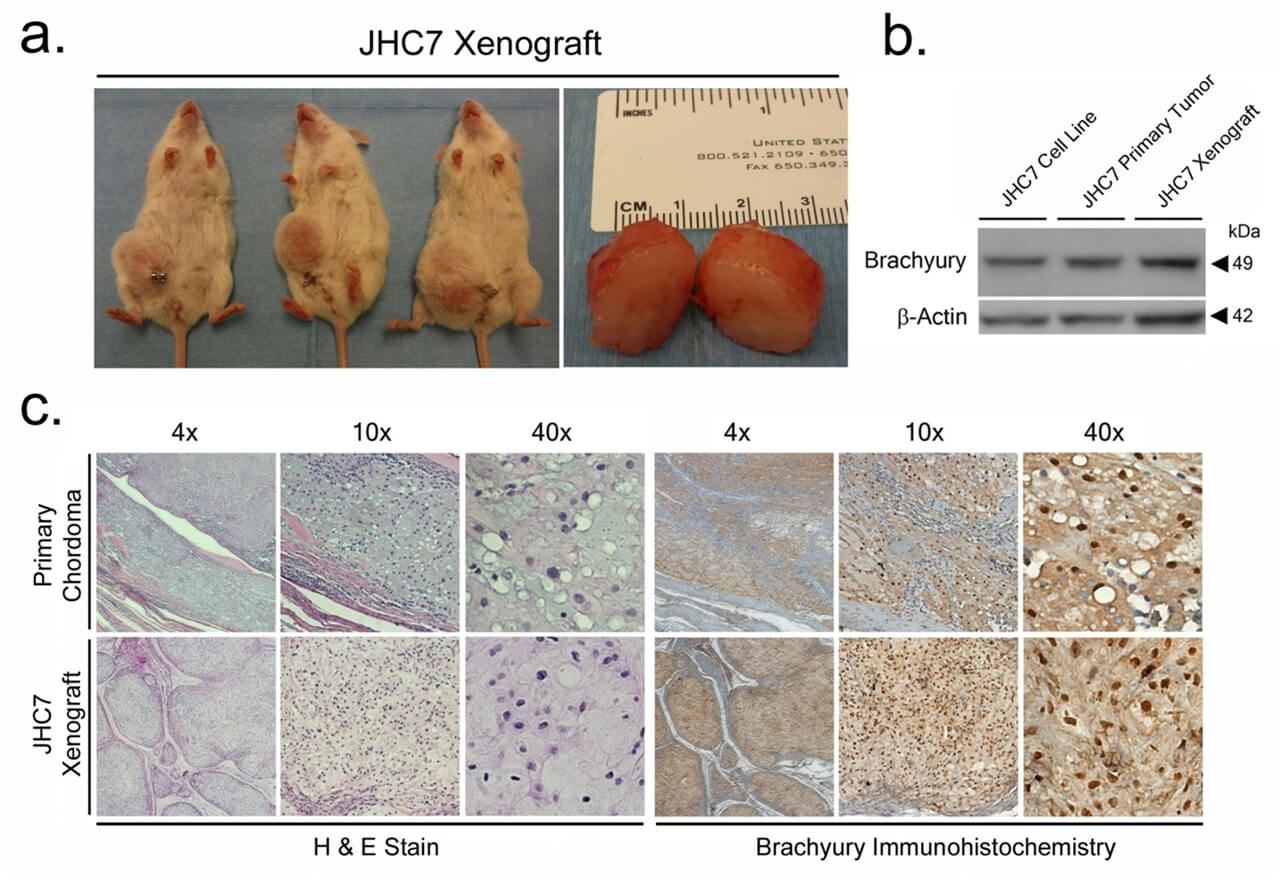
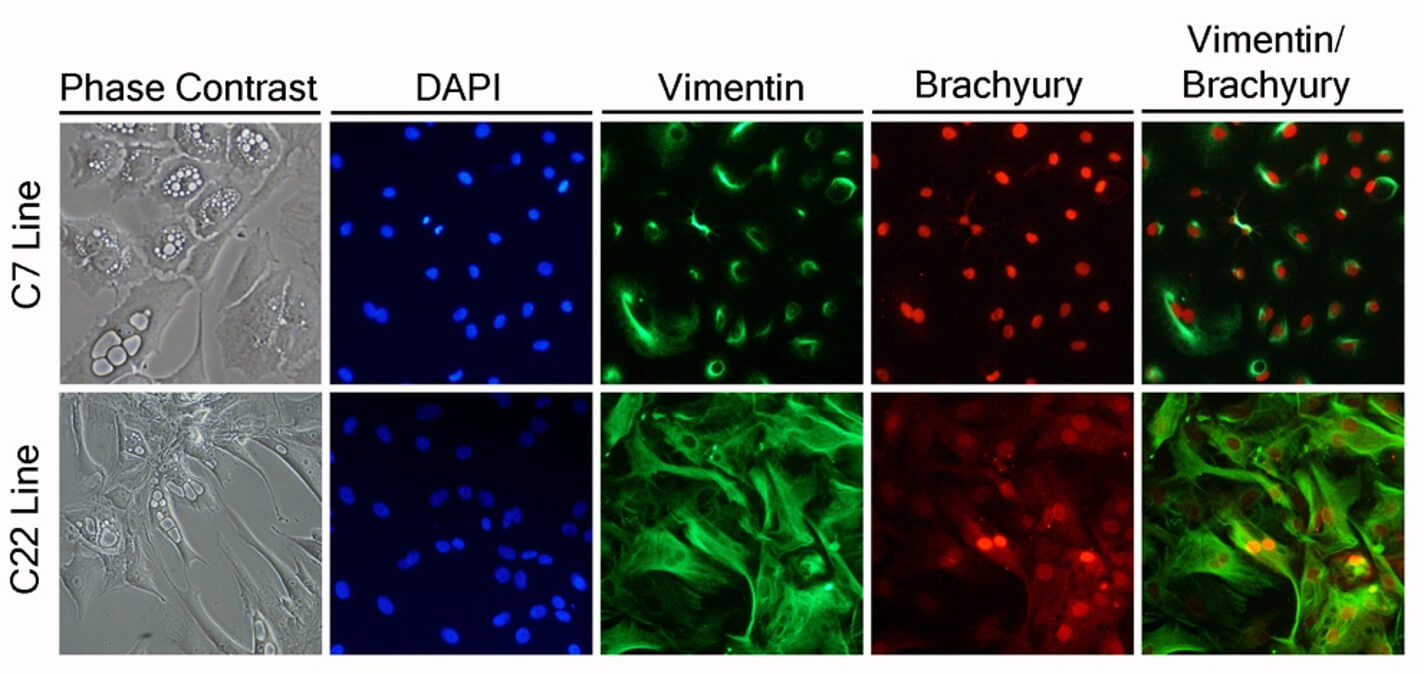 Over the past decade, my research group and I established one of the first human chordoma cell lines in the scientific literature, a key resource that has advanced research in this field. We also developed the first animal chordoma xenograft model and identified brachyury as a major molecular target in arresting disease progression using shRNA and CRISPER knockout strategies as a proof of concept. Brachyury, as a result of this work, has become an attractive molecular target, with multiple national clinical trials focusing on targeting it via immunotherapeutics while other trials focused on small molecule inhibition of this transcription factor. Our team also discovered that many of the transcriptional programs seen in chordoma appear to also be co-opted by glioblastoma and other cancers. This pathway is now implicated in epithelial to mesenchymal transition states of other carcinomas including breast and lung cancer. These discoveries have underscored for our team the utility of the operating room as an extension of our laboratory to accelerate research. Human tissues have directly helped us model these diseases and identify key transcriptional programs that are now targetable.
Over the past decade, my research group and I established one of the first human chordoma cell lines in the scientific literature, a key resource that has advanced research in this field. We also developed the first animal chordoma xenograft model and identified brachyury as a major molecular target in arresting disease progression using shRNA and CRISPER knockout strategies as a proof of concept. Brachyury, as a result of this work, has become an attractive molecular target, with multiple national clinical trials focusing on targeting it via immunotherapeutics while other trials focused on small molecule inhibition of this transcription factor. Our team also discovered that many of the transcriptional programs seen in chordoma appear to also be co-opted by glioblastoma and other cancers. This pathway is now implicated in epithelial to mesenchymal transition states of other carcinomas including breast and lung cancer. These discoveries have underscored for our team the utility of the operating room as an extension of our laboratory to accelerate research. Human tissues have directly helped us model these diseases and identify key transcriptional programs that are now targetable.
Yuki Research Lab
Novel Liquid Embolic System for the treatment of hypervascular tumors and vascular malformations.
Trans-arterial embolization is a procedure used to stop blood flow to specific areas of the body, often to treat abnormal blood vessels or tumors. By inserting a catheter into an artery, small particles, Liquid Embolic Materials (LEMs), or coils are injected to halt blood flow. This procedure is commonly used to reduce bleeding during surgery or to shrink large hypervascular tumors. However, current embolic materials have limitations.
One commonly used embolic material is micro-particles, but they have drawbacks such as limited tissue penetration and poor visibility under X-ray. LEMs offer advantages over micro-particles, including better tissue penetration and permanent vessel closure. However, FDA-approved LEMs like n-butyl cyanoacrylate (nBCA) and Onyx, which contains ethylene vinyl alcohol (EVOH) dissolved in dimethyl sulfoxide (DMSO), aren't suitable for many treatments due to their limitations. nBCA is a strong adhesive with a significant risk of catheter entrapment, and its pro-inflammatory nature is not suited for tumor treatment. Similarly, the organic solvent DMSO used in Onyx carries strong tissue toxicity. Thus, none of the existing LEMs are FDA-approved for treating conditions such as hypervascular tumors or trauma-related vessel injuries.
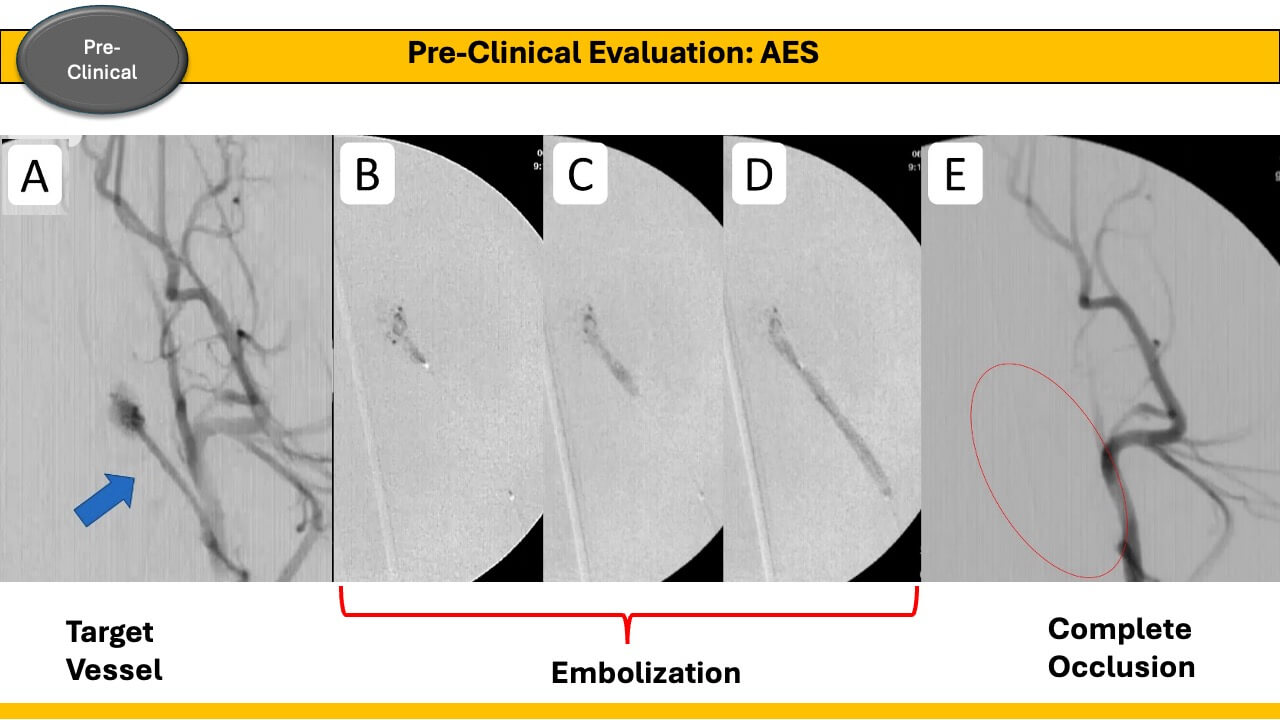
To address this, we developed a novel LEM called Aqua Embolic System (AES), a single-component water-based LEM. AES, made of biocompatible polysaccharides, forms a solid hydrogel cast triggered by blood calcium. It offers excellent tissue penetration, can be delivered with any single-lumen micro-catheter, and contains no toxic solvents like DMSO. AES shows promise for treating vascular malformations or hypervascular tumors, with the potential for delivering multiple chemotherapy agents. The research team includes Dr. Ichiro Yuki, Ms. Parisa Khosropour, Dr. Shuichi Suzuki, and Dr. Frank P.K. Hsu. The material is provided by polymer scientist Dr. Kousaku Ohkawa from the Institute of Fiber Engineering, Shinshu University, Japan.
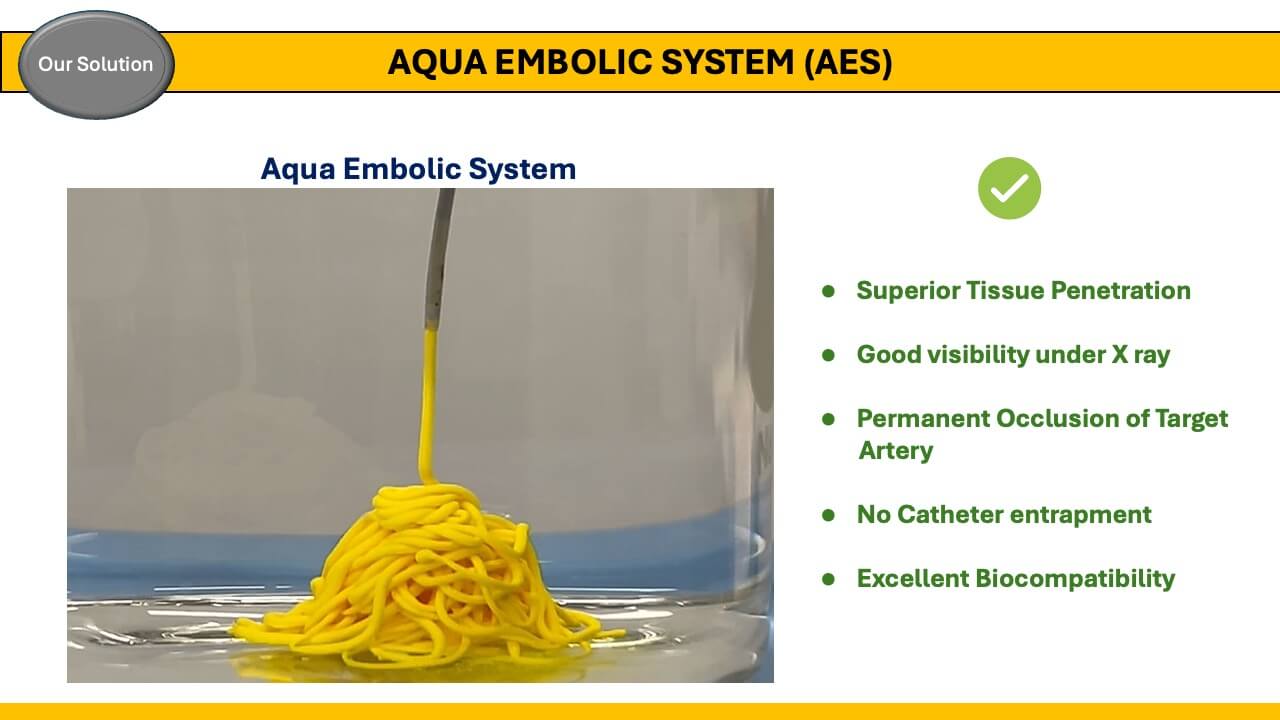
This project has received support from multiple research grants, including the ICTS Grant (2019) by UC Irvine, Proof of Product (POP) Grant (2022) by Beall Applied Innovation, 2 Grants by Japan Society for the Promotion of Science (2015 and 2022), and recently, an NIH Grant (STTR: Small Business Technology Transfer) (2023).
The project is currently undergoing pre-clinical evaluation, followed by clinical evaluations and FDA approval for commercialization.
Jefferson W. Chen, MD, PhD, Normal Pressure Hydrocephalus (NPH)
NPH is a difficult-to-diagnose disorder that occurs mainly in older adults and has three main symptoms: difficulty walking, or gait imbalance; urinary incontinence and memory problems.
One of the most accurate ways to diagnose NPH is to drain small amounts of spinal fluid over the course of three days while the patient performs a series
of tests to examine their gait, cognition and ability to carry out general daily activities.
Patients whose symptoms improve after the spinal drainage have a good
chance for longer term improvement with a permanent brain shunt. Our study aims to determine which factors predict whether a patient improves with a shunt.
Intracranial pressure waveform analysis
This project, conducted in collaboration with the departments of Biomedical Engineering and Neurology, involves gathering data on patients being treated for a variety of conditions, including traumatic brain injury, intracerebral hemorrhage, stroke and subarachnoid hemorrhage.
Any patient who has a tube placed into the brain to monitor intracranial pressure (ICP) is eligible. Physiological data is recorded then analyzed with a sophisticated computer program. By analyzing the ICP waveform, we are working to develop a model that can predict dangerous ICP elevations before they occur and allow intervention in advance.
Brain tumor - Skull base lab
Our faculty members also are active in many areas of basic and clinical research on brain tumors. Recent projects include:
-
Dennis Malkasian, MD, PhD, Director, Skull Base Lab
Educational focus primarily for training residents and post-graduate skull base fellows, a methodological approach.- Post-graduate level lectures and cadaveraic dissections on classical and operative neuroanatomy, skull base anatomy, cervical and intracranial/extracranial surgical anatomy.
- Fundamentals of neurogenesis, morphogenesis, and general structural neural development.
- Relationship between ontogensis and oncogensis
Sumeet Vadera, MD, FACS, FAANS
Dr. Sumeet Vadera has an interest in brain-machine interface research and epilepsy surgery outcomes. He has received several grants including the Epilepsy Foundation Grant and the Medtronic Grant for novel surgical techniques. Dr. Vadera's commitment to research extends beyond conventional boundaries including his interest in improving the value and reducing the cost of care provided.
Michael Oh, MD, Spine Research
Our Spine Team is deeply committed to delivering state-of-the-art treatment for spine-related disorders through compassionate care, a collaborative team of specialists, and the seamless integration of advanced technology. Beyond this primary focus, our dedication extends to pioneering medical advancements through meticulous, inclusive and innovative research endeavors. These initiatives span from enhancing medical education to critically evaluating treatment algorithms.
In the last year, numerous projects by our team have been accepted at national and international conferences including Spine Summit, the Pacific Spine and Pain Society, AANS, and EFORT with additional projects still awaiting review.
NeuroSim: A Portable and Cost-effective Neurological Simulation Device
The demand for simulation devices is on the rise as residency programs adapt to work hour limitations while maintaining resident technical proficiency. Our team has developed a patented training device, utilizing computer-aided design (CAD) modeling to replicate neurosurgical procedures. This simulation tool enriches medical education by providing trainees with opportunities to refine surgical techniques, enhance anatomical knowledge, and develop motor skills with tactile feedback. Its educational efficacy has been validated among medical students and its educational utility has been confirmed through market discovery through UCI’s NSF funded Innovation Corps. Future research efforts will focus on assessing motor skill acquisition with the device.
Perioperative Optimization of Spine Surgery Patients
Complications are an unfortunate reality in surgery despite technical precision. Our team employs large data to identify and evaluate preoperative risk factors associated with adverse outcomes in spine surgery. Through this research, we have identified modifiable risk factors contributing to spine complications and have adjusted our clinical practices accordingly. Leveraging our multidisciplinary expertise, we aim to minimize the likelihood of complications for our patients. Additionally, our team was awarded the 2023 AO Spine Research Start-up Grant to initiate a prospective, randomized, double-blind clinical trial investigating the role of essential amino acids in lumbar decompression surgery. Retrospective studies are currently ongoing to evaluate how the findings from our large data analysis compare to our institutions.
Evaluation of the Treatment Algorithm for Spondylodiscitis
Spondylodiscitis, an infection of the intervertebral disc, poses diagnostic and management challenges. Our systematic literature review revealed improved pathogen identification and reduced pain with percutaneous endoscopic debridement and drainage (PEDD) compared to CT-guided biopsy. These findings have been corroborated in a retrospective case series conducted at our institution. Currently, we are conducting a prospective, randomized, blinded clinical study, funded by the San Diego Spine Foundation, to compare pathogen identification rates and clinical outcomes between CT-guided biopsy and PEDD in the management of spondylodiscitis.
Implementation of Artificial Intelligence to Improve Surgical Outcomes
Artificial intelligence offers the potential to analyze vast datasets and optimize medical care efficiency. Collaborating with computer scientists, our team is developing a predictive model to identify patients at risk of poor outcomes in spine surgery. By providing personalized guidance, we aim to mitigate complications and enhance patient care.
Educational Utility of Augmented and Virtual Reality Models for Patient Education
Augmented and virtual reality models offer a more approachable means to discuss patient pathology. The use of these tools has been described to augment patient education and enhance comprehension of complex spinal anatomy and conditions. Following receipt of the 2022 Pacific Spine and Pain Society Research grant, we evaluated augmented reality models for patient education in the outpatient spine clinic. Our preliminary findings indicate improved patient understanding and preference for augmented reality over traditional imaging modalities. As we continue to expand our research, our goal is to integrate these tools into clinical practice for the benefit of our patients.
Single and Multicenter Retrospective Studies
Comprehensive evaluation of complications, outcomes, and the dissemination of novel findings is paramount in spine care. In collaboration with UCI’s Office of Research Information, we have developed an automated data extraction pipeline, significantly streamlining database creation for our single-center retrospective studies. Moreover, we engage in collaborative projects with academic institutions nationwide, addressing diverse topics such as pelvic fixation strategies and outcomes associated with spinal hardware.
Sponsored Clinical Research Studies
Through strategic partnerships with industry leaders, we offer our patients access to cutting-edge technologies in spine care. Our ongoing clinical studies encompass innovative solutions such as Premia Spine’s TOPS System, Spineart’s BAGUERA C cervical disc replacement, and Medtronic’s Infuse bone graft in Transforaminal Lumbar Interbody Fusion.
For information about other research or collaboration requests, please call 714-456-6966.